Liz Edmonds
Nurse and senior nursing administrator at Footscray Hospital 1960–present
Liz Edmonds grew up in Braybrook and graduated from Sunshine High School.
She enrolled as a student nurse at the hospital’s nurse training school in 1960. After graduating she worked on surgical wards and later became a nursing administrator.
Nurses living, training, working on site
“Students trained on site at the nursing school for three years before graduating. We all had to live in at the nurses’ home, which was a seven-storey building. You started living on the sixth floor as a junior student, then gradually moved down as you became more senior. There were about 20 single bedrooms on each floor, a laundry and small lounge room and kitchen on each floor.
There was a home sister on each floor. Matron Mitchell and the nursing sisters acted as our parents. It made sense because we were young, 17, and our parents had entrusted them with our care.
The nurses’ home was locked at midnight. If you were going to a ball you would have to go to the Matron and ask permission and get a late pass until 1or 2am. When you came back you had to report to the after hours staff.”
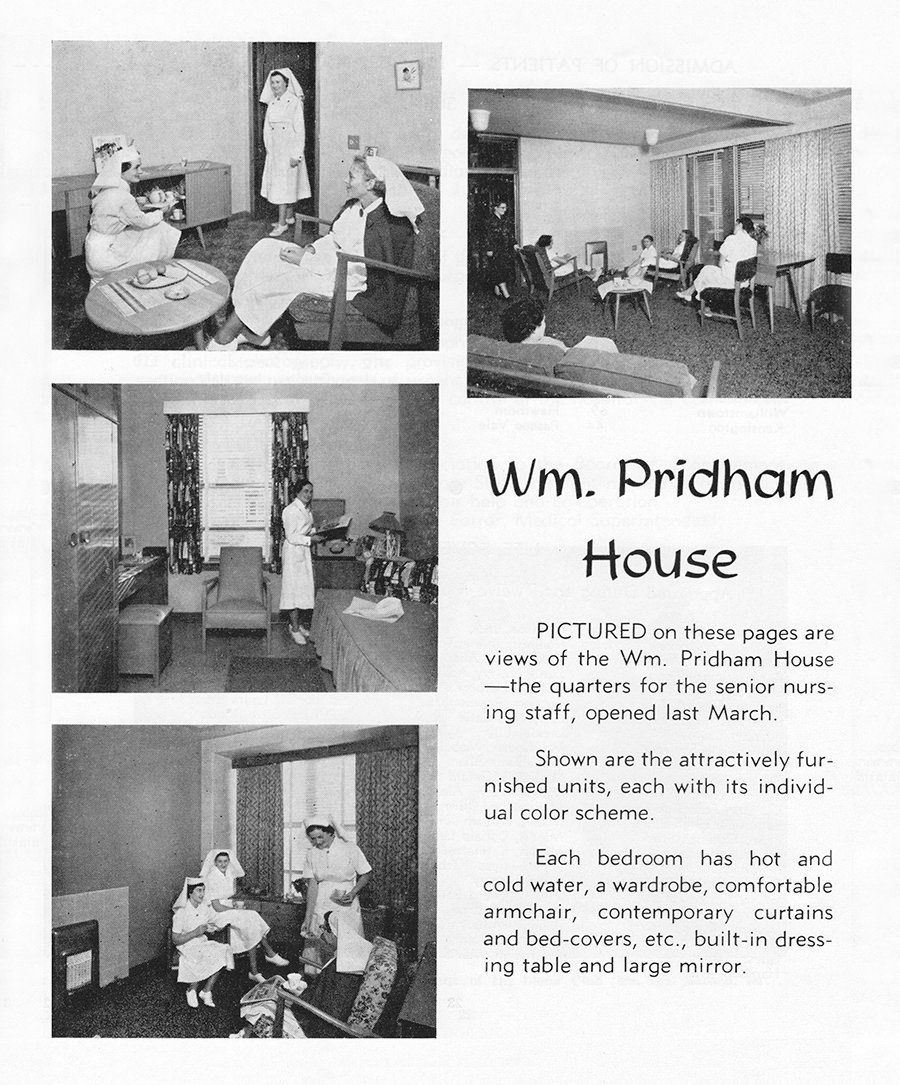
Senior nurses’ quarters at William Pridham House in 1953. The building provided accommodation for 105 nurses.
Western Health archives
Workplace culture in the 1960s
“You never sat in the presence of the senior medical staff. If the surgeons came up to the ward to do their rounds and you were at the staff desk, you stood up. You were told how to behave when you first started and everybody followed those rules.
You never called anybody by their first name. It was very formal. Mr Francis, Matron Mitchell.
Kendall Francis was gorgeous. All of the nurses loved Kendall. He was tall, dark and handsome, friendly, not moody. A lot of surgeons can be moody and have an arrogant way about them but Kendall wasn’t like that.
Conrad Ley was a tall, domineering sort of man who used to frighten the wits out of people. You went to theatre in your second year and everybody told me Conrad will yell at you and try and upset you and make you cry.
I thought ‘there’s no way he’s going to make me cry’. So every time he yelled at me, I laughed. He would look at me strangely but we ended up getting on very well because he saw I wasn’t going to burst into tears. It was a bit like a right of passage that you had to get past.
Some of the surgeons were awful in those days – they would throw things. If they got handed the wrong instrument in theatre, some of them would fling it across the room. That was rare but it happened.
The surgeons were all honorary then and they weren’t paid for their public patients and there were more private patients then.
People had to pay to visit their relatives as private patients. You had an orderly standing at the door and you had to pay with a silver coin to go in and visit the patient in the 60s. It was very rigid. Only two visitors at a time and no children allowed.
I stopped working when I had my first child. They wouldn’t take part time nurses so I didn’t go back to work until after I had my second child. When I returned in 1968, workplace culture had really changed because everybody, except for the senior medical staff – was calling each other by their first names. That was a real shock to me: that this had happened over about three years, that the culture had changed so quickly.”
How patients changed
“Before the liquor licencing laws were changed, and drink driving and seat belt laws were brought in during the late 60s and early 70s, we had a much younger patient population. We used to get the most appalling traumas, shocking head injuries, multiple traumas. The surgeons would be trying to put those people back together.
Hotels used to shut at 6 o’clock. It was called the 6 o’clock swill, where people would get blind drunk on their way home from work and prang their cars.
I worked in the emergency department in the mid 70s. The horrendous trauma cases had a huge impact on the wards because some of these people lived forever even though they were virtually vegetables and they’d be specialled and took up beds for so long.
So our patient population was much younger. The workload for our senior medical staff was huge because there was so much responsibility that rested only on their shoulders, whereas now the workload is spread because surgeons have decent numbers of registrar staff.
The reality is that if you’ve got good people on the floor at registrar level who you know can handle things, you don’t have to sleep with one eye open all the time. Particularly for the general surgeons, who have to be ready to come in within an hour.”
How surgery changed
“There have been huge changes in an area like orthopaedics. In the early years if a patient had a neck of femur fracture – I never saw them walk again. People stayed in hospital so long and the practice wasn’t to get people out of bed.
The removal of a gall bag – cholecystectomy – used to involve opening the abdomen and the patient would be in hospital for 10 days, now the patient goes home the next day.
It’s much less common now that surgical patients need blood transfusions during surgery because of the greater efficiency and advances in surgical practices, techniques and technology.
Pain management in surgery has changed dramatically. I still have memories of people being in absolute agony. Pain management is so much better and it’s a specialty in its own right, associated with the anaesthetics department.
I still have nightmares sometimes when I think of people who were dying of cancer who could only have their narcotic every four hours. You would ring and ask if you could have more but everybody was so frightened of killing people with narcotics then.
We now have nursing specialties that pick up the things that surgeons can’t do or don’t have time to do. We have breast care nurses, stomal therapists, the acute pain nurses and intensive care liaison nurses. Now there’s a lot of nursing expertise in addition to the nurses and doctors on the floor.
The senior medical staff are very appreciative of that because they know it’s evidence-based, best care for their patients. For example the colorectal surgeons love the stomal therapist because they wouldn’t be able to manage their patients without her. She’s got the time to make sure that patients can manage their colostomy bag and make sure they get the supplies they need – all those things that busy surgeons or interns wouldn’t know how to access. That group of nurses are a very integral part of the surgical team.”
Fundraising, community ties
“As student nurses we were encouraged to fund raise for the hospital and we had competitions among the different intake groups of nurses as to who could raise the most funds.”

Miss Footscray Hospital, Pam Mayall, is crowned Queen of Industry in the 1963 Queen of Industry Quest conducted by the Lions Club of Footscray. The runners-up are Miss Exchange Hotel, Diane McKechnie, (left) and Miss Colonial Sugar Refineries, Dellis Kaye.
Western Health archives

