The honorary system for surgeons in public hospitals had no chance of withstanding the demographic, technological and political changes sweeping through Australia in the 1970s.
At a national level, the Whitlam government’s election in 1972 ushered in a healthcare revolution.
The government introduced Medibank, the nation’s first universal health-insurance scheme, which gave Australians free treatment at public hospitals and for medical services regardless of their financial status.
Patients no longer had to pay a fee to be treated for emergency, outpatient medical services and in-patient care.
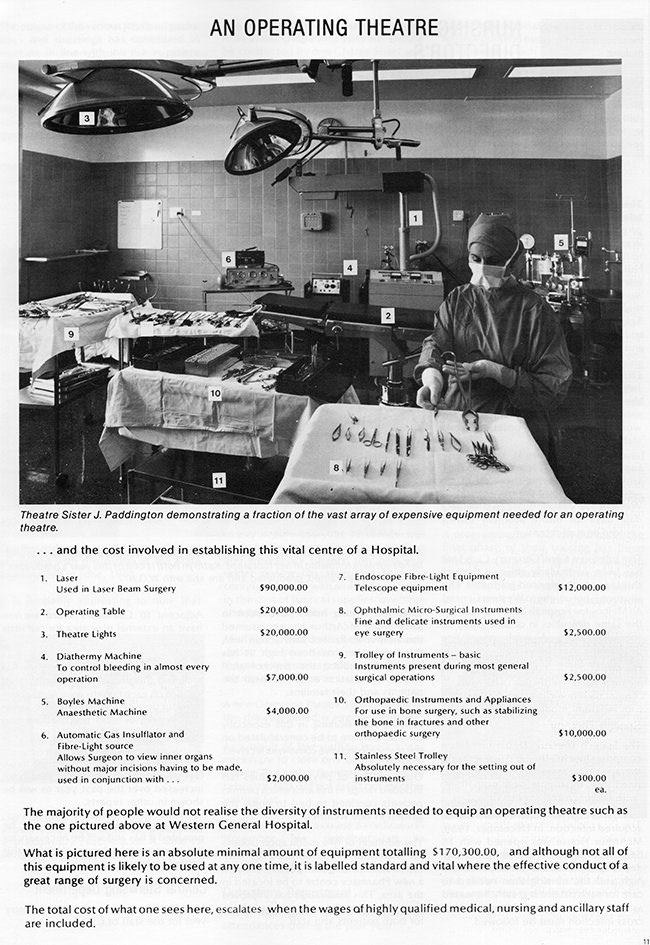
The government embarked on a massive expansion of Australia’s health services, pouring money into new hospital facilities, especially in the rapidly expanding suburbs of the nation’s cities.
It introduced a Medibank levy that provided an extra funding stream for cash-strapped hospitals.
It struck hospital agreements with state governments and dispensed Commonwealth grants equal to 50 per cent of net operating public hospital costs. The grants put hospitals on a more secure financial footing and reduced their reliance on parsimonious state organisations such as Victoria’s Hospital and Charities Board.
When Gough Whitlam died on 21 October 2014, Bob Hawke, another former Labor Prime Minister, spoke of Whitlam’s legacy and Medibank’s immediate impact on the lives of ordinary people.
“Before Medibank the prospect of sickness, ill health and hospitalisation caused poorer people to face the prospect of financial and personal disaster,” Mr Hawke said. “The national health scheme was arguably one of the best and fairest in the world.”