Medical staff ate their daily meals in formal splendour at the hospital until the 70s. There were two dining rooms – one for doctors and a larger room for nurses and the rest of the hospital staff including orderlies, pathology and radiology.
Staff were served at lunch and dinner by a maître d’ and waitresses dressed in black skirts, white aprons and white shirts. The tables were set with silverware and linen tablecloths.
A late supper – a cooked meal – was served at 11.30pm for staff on the night shift.
“Everyone ate in the dining room,” said theatre nurse Beverly Howard, who joined the hospital in 1963 as a student nurse. “ Morning and afternoon tea were also supplied. They were fabulous - all home cooked. And on Christmas Day the residents and registrars would all dress up and wait on tables, looking after the nurses. It was great fun. In those days the hospital was like one big family – everyone knew everyone else.”
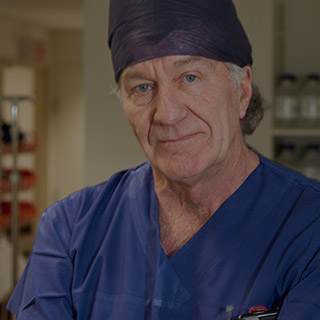
The dining rituals of the hospital’s early decades reflected the structures of power within the organisation. The surgeons and their fellow medical clinicians were the hospital’s leaders, wielding enormous influence on the small team of administrators, according to Bob Thomas, the hospital’s first Professor of Surgery.
“In the early days, surgeons had to deal with a huge variety of cases and that’s what created the characters of that era – in the crucible of fire type of people, people who dealt with multi-traumas,” Professor Thomas said.